TUSCALOOSA, Ala. — Researchers at The University of Alabama identified a critical mechanism for how signals from the environment are integrated with genetic information to influence the health and survival of brain cells, providing a key insight into the development of Parkinson’s disease.
In findings outlined in a paper recently published in the Proceedings of the National Academy of Sciences, researchers open unexplored treatment avenues that could emphasize how regulation of forces outside the body contribute to the protection of brain cells, or neurons.
“This is not instantly a magic bullet, but this work tells us a lot about new possibilities for therapies,” said Dr. Guy Caldwell, University Distinguished Research Professor in biological sciences, whose lab led the research. “We showed solid evidence on how this combination genetic-and-environmental mechanism influences neurodegeneration, but how to exploit it is the next area of discovery.”
Currently, no cure or treatment exists to prevent or halt this disease that affects more than 10 million people globally, with more than 60,000 Americans diagnosed annually. The recent study examined neurons that produce the chemical dopamine. Progressive death of dopamine neurons underlies the onset and symptoms commonly associated with Parkinson’s disease, such as tremor and involuntary shakes. When a Parkinson’s patient begins to exhibit symptoms of the disease, they have likely lost up to 50 to 80% of the dopamine neurons in their bodies.
This new research shows how a specific protein in the body, TNK2, acts as a sort of dial, turning up or down the use of certain genes, effectively tuning dopamine levels to optimize neuron function and survival. In contrast, mutations in the human TNK2 gene result in the degeneration of dopamine-producing neurons, leading to Parkinson’s.
Caldwell, Dr. Kim Caldwell, professor of biological sciences, and Dr. Han-A Park, assistant professor of human nutrition, and six UA students co-authored the paper in PNAS, a highly respected academic journal.
The Caldwells’ lab received funding from the National Institutes of Health to identify molecular factors that influence whether an individual is either resilient or susceptible to dopamine neuron degeneration. The research delves into epigenetics, the study of mechanisms that switch on and off genes in response to outside environmental stressors.
The UA researchers report the discovery of an intersection where the control of dopamine levels and regulation of epigenetic response meet to confer their combined impact on neuron health. Given the variety of important biological functions and behaviors involving dopamine, the implications of this research include potential ways to influence wide-ranging conditions, from depression and schizophrenia to addiction and Parkinson’s.

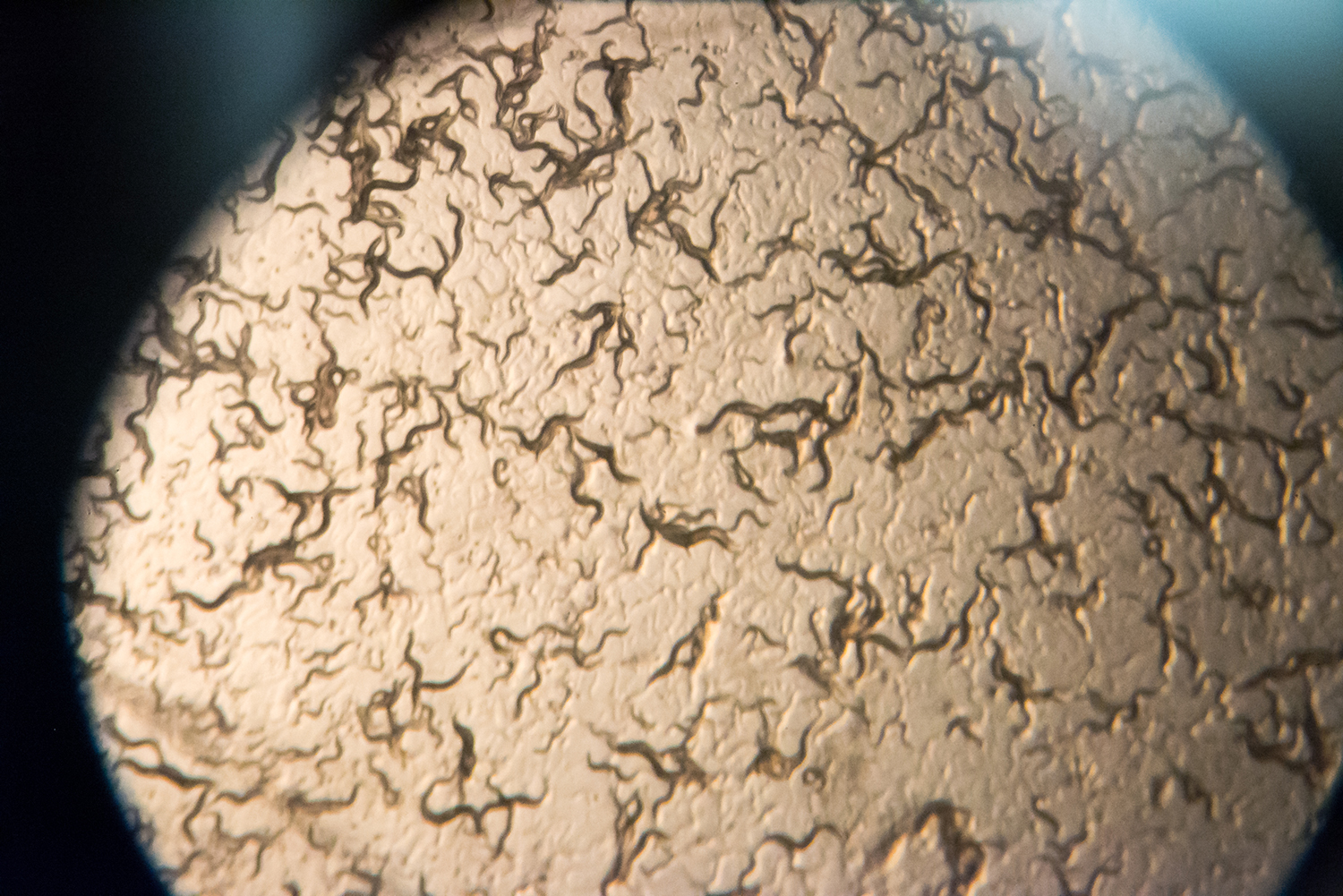
For this study, researchers altered genes of tiny roundworms known as C. elegans, mimicking the mutations found in patients. The worms share roughly half their genes with humans, and their basic features allow inexpensive and rapid experimentation for a range of neurological diseases. UA researchers can induce Parkinson’s-like effects in the worm’s dopamine neurons, as a proxy for testing the loss of neurons in the human brain as part of the disease.
Prior findings using the Caldwells’ worm models have repeatedly led to results later validated in human research, and the study discussed in the paper is another strong endorsement of the worm as a preclinical model for neurodegenerative disease research.
“This research shows how we can use a system like worms to decipher the meaning of genetic variations in humans,” Caldwell said. “With the growing informational overload of human DNA sequencing data that exists, parsing ‘the music within the noise’ is essential for the proper interpretation of the many differences between all of us.”
Although the worm’s version of human TNK2, named SID-3, is slightly different, it controls dopamine levels in the worms the same way as TNK2 in humans. The human protein TNK2 is known to help bring and recycle dopamine into neurons, whereas SID-3 in worms is known to regulate the transport of snippets of a type of small, traveling, double-stranded RNA molecules called microRNAs that act in response to environmental changes and determine whether genes are expressed.
When the TNK2 protein is mutated, as found in Parkinson’s patients, it delivers an excess of microRNA, continuously suppressing genes that normally maintain the balance of dopamine in dopamine neurons. This also results in TNK2 simultaneously recycling too much dopamine, removing dopamine from the space between neurons, called a synapse, where it is needed.
This combination of depleting synaptic dopamine, while suppressing genes involved in neuroprotection, explains why patients with TNK2 mutations exhibit Parkinson’s. The study directly demonstrated the mutated protein stays active too long, robbing the neurons of the dopamine balance needed for normal function.
“Dopamine is tightly regulated within the body, and a little tweak of dopamine levels can have a profound impact. By engineering worms to mimic the patient mutations, we clarified that the TNK2 protein is staying on too long,” Caldwell said. “The ‘dial’ is not responding to being turned and is not behaving like it should be, and that imbalance leads to neurodegeneration.”
Park, the assistant professor of human nutrition, and her student, Madison Scott, showed the same mechanism for regulating TNK2 levels was present in neurons cultured in a lab from rats. This extended the significance of the worm findings to mammals and hints at future research being fruitful.
Along with professors Caldwell and Park, other co-authors on the paper include recent UA graduate students Brucker Nourse and Shannon Russell, former UA undergraduates Nathan Moniz and Madison Scott, along with current undergraduates Kylie Peter and Lena Seyfarth.
Contact
Adam Jones, UA Strategic Communications, 205-348-4328, adam.jones@ua.edu