
A drop in blood glucose levels in the middle of the night can increase the risk of hypoglycemia, which can cause a range of symptoms that can linger throughout an entire morning.
It can also cause a medical emergency if blood glucose levels aren’t regulated immediately.
When University of Alabama alumna and Huntsville native Dana Lewis was an undergraduate student living in Riverside Hall, she used a blood glucose monitor and an insulin pump to control her Type 1 diabetes throughout the day and night. Diagnosed at 14, she was used to monitoring her levels and adjusting her daily and nightly routines to stay in optimal range. That process also includes the continuous glucose monitor’s alarm system that notifies the patient when ranges are too low or too high. However, the alarm wasn’t loud enough for Lewis, who would routinely sleep through it.
Lewis’ remedy for missing alarms was to routinely check in with her mother, whom she would text whenever she woke in the morning.
“One night, my phone wasn’t plugged in all the way and died,” Lewis said. “My mother couldn’t reach me and started to worry because all of her calls went straight to voicemail. Everything was fine, and I called her when I woke up, but it was a reminder of how real that safety mechanism is for her and me, and saying, ‘this is not good enough.’”
Lewis began brainstorming ways to transfer data from her monitor to a phone or computer to make louder alarms that would actually wake her up, but the technology wasn’t available to fully conceptualize it and build it. A few years after Lewis graduated from UA in 2010 and moved to Seattle, Washington — thanks to others who figured out how to access data from the continuous glucose monitor — she then figured out how to display her blood sugar data on a web page and create a system in which, if she didn’t take action when notified of low blood sugar levels, her family would be notified.
She now had a louder alarm, and her family had peace of mind and a better understanding of how her levels varied at different times of the day.
The artificial pancreas
Lewis majored in public relations and political science at UA and was enrolled in the Computer-Based Honors Program, where she learned two coding languages – C++ and FORTRAN 90 – during her first year.

The idea of CBHP is to give students a foundation for learning other programming languages and to begin undergraduate research their second year. Lewis didn’t know it at the time, but she’d later apply those skills to a field she never imagined she’d work: medical technology development.
“Because we had built this multi-level system with alarms, we were able to take this data and build a predictive algorithm that would take real-time data and predict the future levels of blood sugar,” Lewis said. “Essentially, ‘you’re going to go low or high, but if you take action now, that high or low will be less severe.’ A couple of months later, we met and worked with someone who had figured out how to communicate directly with the insulin pump, and at that point, it was easy to take that piece, plug into our system, and that’s how we ended up with what we call the ‘artificial pancreas.’”
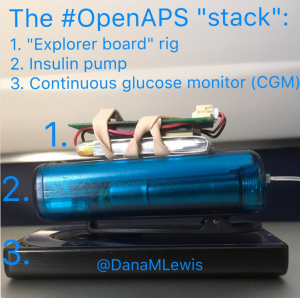
The Open Source Artificial Pancreas System (OpenAPS) works by running the data from the monitor through the algorithm, and then communicating decisions back to the insulin pump every five minutes. The hardware – roughly the size of two containers of lip protectant – works wirelessly and can be clipped to clothing or kept in a pocket or nearby. Data can also be linked to and displayed on a cell phone.
“If I’m traveling by myself and my blood sugar starts dropping, my husband can look at it,” Lewis said. “It’s awesome to have remote visibility into what’s happening and not have to be physically near the person and press the buttons on their device to see what’s happening.”
All the code, documentation and reference guides are open-sourced materials available online so that other people who have compatible devices could build the system themselves. Lewis said roughly 300 people around the world have either built their own or are at some point of development, which has grown a network of people who help each other troubleshoot and continue to improve the system.
“I don’t regret for a second making our work open source because that’s 300 people whose lives are changed, and I’d much rather have done that, even though there’s going to be commercial options coming into the market in a couple of years,” Lewis said. “That’s many, many days of kids who can go to school and just be kids, and parents who don’t worry about their kids, and adults who are able to live their lives. We could have maybe made money, but all the money in the world is not worth being able to say, ‘I’ve changed one, let alone 300 other people’s lives.’”
Inspiration from home
Though Lewis’ initial plan was to create a louder alarm, her CBHP background rooted her confidence in coding to eventually grow and marry the technology with other devices, and ultimately, have an impact on the people in her home state.

Lewis said she learned about CBHP from her brother, Drew, a UA alumnus and former UA professor who was enrolled in the program. However, she didn’t have engineering or software development aspirations when she enrolled.
“I had a generalist mindset,” Lewis said. “My day job after graduating was focusing on technology and communications in health care. I don’t look like a traditional programmer or developer, and when we first started, I observed a lot of people who said ‘I can’t do this because I don’t have a background.’ CBHP gave me the confidence to actually do all of this and also push back on people and say, ‘neither do I.’ I have a little bit of experience from years ago, but it’s about having the willingness to try and the confidence to learn more.”
Lewis said a path to commercialization would have taken nearly five years, as clinical trials, approvals and regulations are tedious processes in medicine. It also would have kept her technology from having an impact on the human condition until every hurdle was cleared.
She hopes their decision to open-source the blueprint for the artificial pancreas helps start a broader trend of people doing the same for those living with other chronic conditions.
“I am so proud to be from Alabama, and to have graduated from The University of Alabama,” Lewis said. “I don’t know that I’d be where I am without having that combination of experiences, including through the Computer-Based Honors Program. If anything, I hope that, people hearing my story and knowing I’m from Alabama, appreciate all the amazing things coming out of our state and people who graduate from our university.”
