
A snake’s unique ability to change its organs could hold clues for treating human diseases
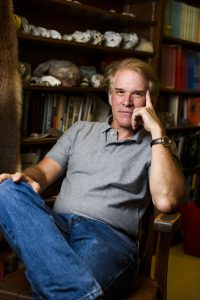
It’s been nearly 25 years since Dr. Stephen Secor discovered the Burmese python’s potential impact on human medicine.
The python is able to grow the microvilli – small, finger-like extensions of cells – in its intestine after each meal, dramatically increasing intestinal surface area for digestion. The greater the surface area, the greater the ability to digest and absorb food, Secor says.
“No other animal had ever been observed to do this, and thus there’s no explanation for it,” Secor says. “I said ‘I want to learn why and how that happens.’”
Secor later developed a model for studying intestinal remodeling in pythons. Initially, the technology was not sufficiently advanced to comprehensively study the underlying changes in intestinal gene and protein expression in the new model.
Secor, now a biology professor at The University of Alabama, focused his earlier efforts on exploring the evolutionary forces that allow pythons, boas and rattlesnakes to remodel their intestines with each meal. Many snakes and other animals do not remodel their intestines.
However, with the recent technological advances to broadly identify changes in gene and protein expression and the collaborative publishing of the Burmese python genome, Secor and colleagues at the University of Texas at Arlington are now focusing on deciphering the molecular mechanisms of intestinal remodeling.
The group will compare tissue, cellular and molecular responses of various snakes, the alligator and rat to gain insight into the underlying mechanism of intestinal restructuring, which could potentially lead to treatments of intestinal diseases.
“What we propose to do, nobody’s done,” Secor said. “While other researchers have examined specific elements on a single species, we’re working with multiple species and undertaking a very broad and integrative approach.”
The approach includes morphology, histology, tissue function, cellular replication, protein expression (proteomics) and gene expression (transcriptomics).
They are studying animals, with a known evolutionary history, that exhibit different intestinal responses to feeding, he said.
“Therefore, we hope to begin mapping the evolution of intestinal remodeling and understand the potential for microvillus lengthening in other animals, including people,” Secor said.
SNAKES!

For much of his career in academia, Secor has studied the biological and physiological phenomena of snakes.
Snakes are uncommon model species for studies aimed at improving the human condition. Previously, Secor struggled to convince biomedical researchers of the viability of using python tissues, as they worked strictly with mammals, mostly mice and rats.
Secor would present evidence that pythons could remodel all of their organs – hearts, kidneys, pancreases, livers and intestines – in a matter of days, whereas humans would take months or even a year.
“It’s a model of extreme physiology, because they undergo the fastest and largest change in mass and function in these organs that anyone has ever seen before,” Secor said.
It’s thought pythons, with feeding, release a blood-borne factor that circulates in their body and triggers the growth of organs, Secor said. In a 2011 article in Science, Secor and colleagues reported that after exposure to plasma from recently fed pythons (but not fasted snakes), heart cells of young rats would increase in size by 70 percent.
Secor is now undertaking a study with possible implications for the future treatment of diabetes in humans. Working with researchers at the Broad Institute in Cambridge, Massachusetts, it was found that plasma from fed pythons will also induce the growth of human pancreatic beta cells and increase their insulin production.
This finding led Secor and his Broad colleagues to study the pancreatic beta cells of four snake species, two of which double pancreas size with feeding and two species that do not.
The goals include identifying the genes responsible for the remodeling pancreatic beta cells in snakes and for humans exposed to python plasma, and to screen for the bloodborne factor that induces beta cell growth. Since failing beta cells are a primary factor in the development of type 1 and 2 diabetes, there is potential for developing a new therapeutic approach to combat diabetes.
“Yes, it is certainly a weird concept,” Secor said, “but there was precedence.”
Researchers had previously replicated a peptide found in the saliva of the Gila Monster, a venomous lizard, into a synthetic form that is the active ingredient in the type 2 diabetes drug, Byetta.
WORK AHEAD
Secor is collecting tissues and plasma to send to colleagues. Snakes will be sent to the Broad Institute this spring, where Secor will be on sabbatical. There, Secor will isolate islet cells from the snakes’ pancreases to examine changes in gene expression of individual cells.
“We will be using a new cutting-edge system for single cell transcriptomics,” Secor said. “It will provide us with a tremendous amount of information from thousands of individual cells.”
Secor said he’s eager to further the work of comparative physiologist Frances G. Benedict, who studied, among other things, the physiology of pythons and boas, and who proposed the value of pythons as a model for biomedical research in the 1930s.
“Benedict’s work with snakes remained absent from textbooks, until our work supported his findings and brought the amazing physiology of these snakes to a larger audience,” Secor said. “The next five years will be exciting. We believe there will be new discoveries that will spark further exploration into the amazing physiology of these animals.”
Dr. Secor’s work with UT-Arlington is supported by the National Science Foundation, and his collaboration with the Broad Institute is supported by a National Institute of Health Transformative Research Award.
